Recent Posts
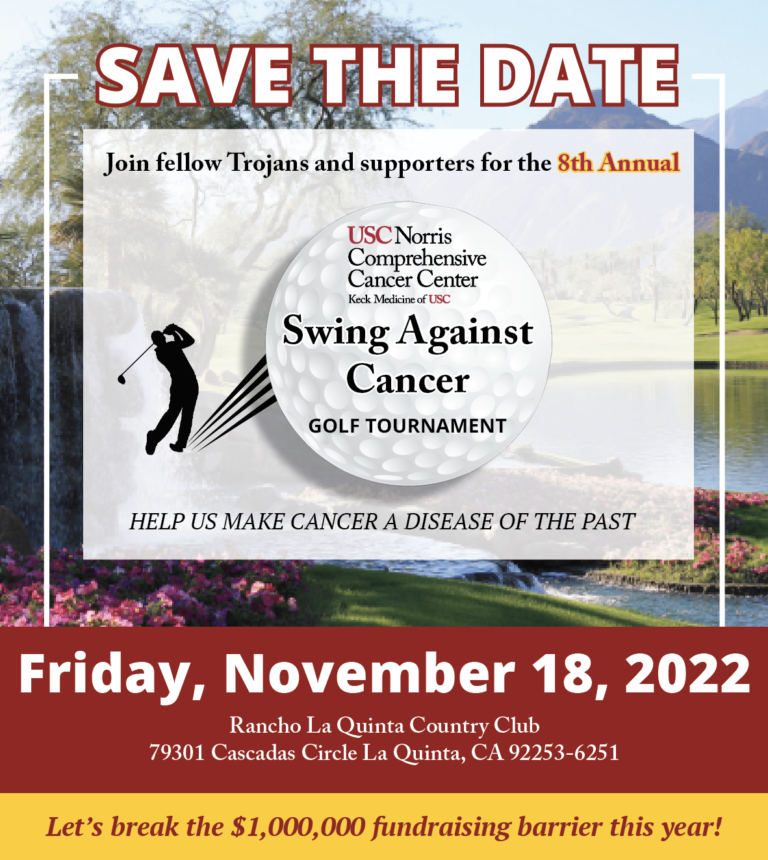
- Swing Against Cancer 2025
- New grant funds first-of-its-kind gene therapy to treat aggressive brain cancer
- Study links PFAS contamination of drinking water to a range of rare cancers
- USC study explores new insights into innate resistance for immunotherapies in colorectal cancer
- An early blood test can predict survival in patients with metastatic prostate cancer, shows USC study
USC Norris shares $500,000 federal grant with Chinatown Service Center to improve equity in cervical cancer screening and treatment
USC Norris Comprehensive Cancer Center is taking part in a new program launched by the Department of Health and Human Services to improve access to cancer care by partnering NCI designated cancer centers with community health centers across the country.
By Hinde Kast
October 19, 2022
 Due to the HPV vaccine and screenings, the vast majority of cervical cancers are preventable. Yet each year 13,000 women are diagnosed with cervical cancer and 4,000 women die from the disease in the United States, according to the Centers for Disease Control and Prevention. In Los Angeles County, racial/ethnic minorities and other marginalized groups, including Chinese Americans and Latinas, are more likely to be diagnosed with cervical cancer.
Due to the HPV vaccine and screenings, the vast majority of cervical cancers are preventable. Yet each year 13,000 women are diagnosed with cervical cancer and 4,000 women die from the disease in the United States, according to the Centers for Disease Control and Prevention. In Los Angeles County, racial/ethnic minorities and other marginalized groups, including Chinese Americans and Latinas, are more likely to be diagnosed with cervical cancer.
To address this disparity, the USC Norris Comprehensive Cancer Center (USC Norris) is joining forces with the Chinatown Service Center to improve access to life-saving cervical cancer screenings, referrals, and treatment for Chinese and Latina women in Central Los Angeles. This first-of-its-kind partnership is part of a new program just launched by the U.S. Department of Health and Human Services’ Health Resources and Services Administration (HRSA) to promote equitable access to cancer screenings and care by bringing community health centers together with National Cancer Institute (NCI)-Designated Cancer Centers. The Chinatown Service Center is one of 11 community health centers across the country sharing a $5 million award from HRSA to implement the new partnerships — and it is the only one in Los Angeles.
“I am extremely excited by the partnership between USC Norris and the Chinatown Service Center and the initiatives that will be developed and implemented to find ways to optimize access, shorten the time frame between diagnosis and treatment, and enhance the quality and delivery of screening and follow up to abnormal findings for cervical cancer patients in our catchment area,” said Dr. Caryn Lerman, director of USC Norris, H. Leslie Hoffman and Elaine S. Hoffman Chair in Cancer Research and associate dean for cancer programs. “We hope to become a model for the nation on how this innovative work can be done to improve cancer outcomes and quality of life for cancer patients and their families.”
USC Norris efforts will be led by Jennifer Tsui, Ph.D., MPH, a member of the USC Norris Cancer Control Research Program and associate professor at the Keck School of Medicine’s Department of Population and Public Health Sciences. The team also includes two additional USC Norris members, Lourdes Baezconde-Garbanati, Ph.D., associate director for community outreach and engagement for USC Norris, and Chanita Hughes- Halbert, Ph.D.,associate director for cancer equity for USC Norris.
“Cervical cancer is a highly preventable disease, but the disproportionate burden of this cancer still rests on racial/ethnic minorities and other marginalized groups, including Chinese American and Latinx communities in Los Angeles,” said Dr. Tsui. “This HRSA-supported project with the Chinatown Service Center will play an instrumental role in facilitating improvement in access to cancer screenings and access to follow-up care while addressing social determinants of health, cultural influences, and structural health system barriers that lead to poor outcomes.”
Cervical cancer death rates within Los Angeles are nearly five times the rate of those in the county, state, and nation. Ensuriing that vulnerable communities have access to HPV vaccines and early detection/screening strategies, which prevent 93% of cervical cancers, is vital to bringing the cervical cancer death rate down in the city.
“The partnership between the Chinatown Service Center and USC Norris supported by HRSA is truly a game changer,” said Dr. Baezconde-Garbanati, a professor in the Department of Population and Public Health Sciences at the Keck School of Medicine. “Not only will this effort eliminate disparities, but it will help save lives. This grant will support significant systemic changes to accelerate the integration of traditionally medically underserved disadvantaged communities in Los Angeles into treatment, optimizing access, and shortening the time between screening, diagnosis, and follow-up care. We are delighted to join our Chinatown Service Center partners in this significant venture. “
To maximize equitable access to cervical cancer screening and treatment, the USC Norris cancer center and the Chinatown Service Center will work together to address barriers to equitable care by providing community outreach and patient education, training staff in cultural competency practices, especially for the female perspective; guiding patients through the treatment process; establishing referral pathways to ensure follow-up for abnormal screenings; establishing systems to assist patients in adhering to ongoing treatments; providing printed and electronic educational materials in culturally and language specific ways; and providing training in cervical cancer prevention and treatment so the support staff is equipped to provide education in the community.
“We are excited about the partnership between the Chinatown Service Center and USC Norris,” said Dr. Hughes-Halbert, vice chair for research and professor at the Department of Population and Public Health Sciences. “The investment made by HRSA to support cancer screening through collaborative partnerships between Federally Qualified Health Centers (FQHC) and NCI-designated cancer centers leverages the resources and assets in these settings. Working together to address key drivers of disparities at system, provider, and patient levels will bring us closer to cancer health equity.”
Founded in 1971, the Chinatown Service Center is one of the largest community-based Chinese- American organizations in Southern California. As a multi-service, non-profit community health center with FQHC designation, they care for underserved populations at their five clinic sites across Los Angeles County. At these sites, the Chinatown Service Center provides health, dental, and behavioral health services to diverse, immigrant, limited English speaking, and low-income populations. In addition to their community health centers, they also operate a youth center and social service offices, as well as provide economic development services.
“Chinatown Service Center is grateful to HRSA for the opportunity to work alongside the USC Norris Comprehensive Cancer Center to help strengthen our tools to fight and prevent cancer,” said Jack Cheng, chief operating officer at the Chinatown Service Center. “We are so thrilled for this innovative partnership and what it will bring to the underserved patients in our community.”
This investment from the U.S. Department of Health and Human Services, through HRSA, supports President Biden’s Cancer Moonshot Initiative and advances President Biden’s Cancer Moonshot goals, which aim to close the cancer screening gap, decrease the impact of preventable cancers, and support patients and caregivers.
About USC Norris Comprehensive Cancer Center
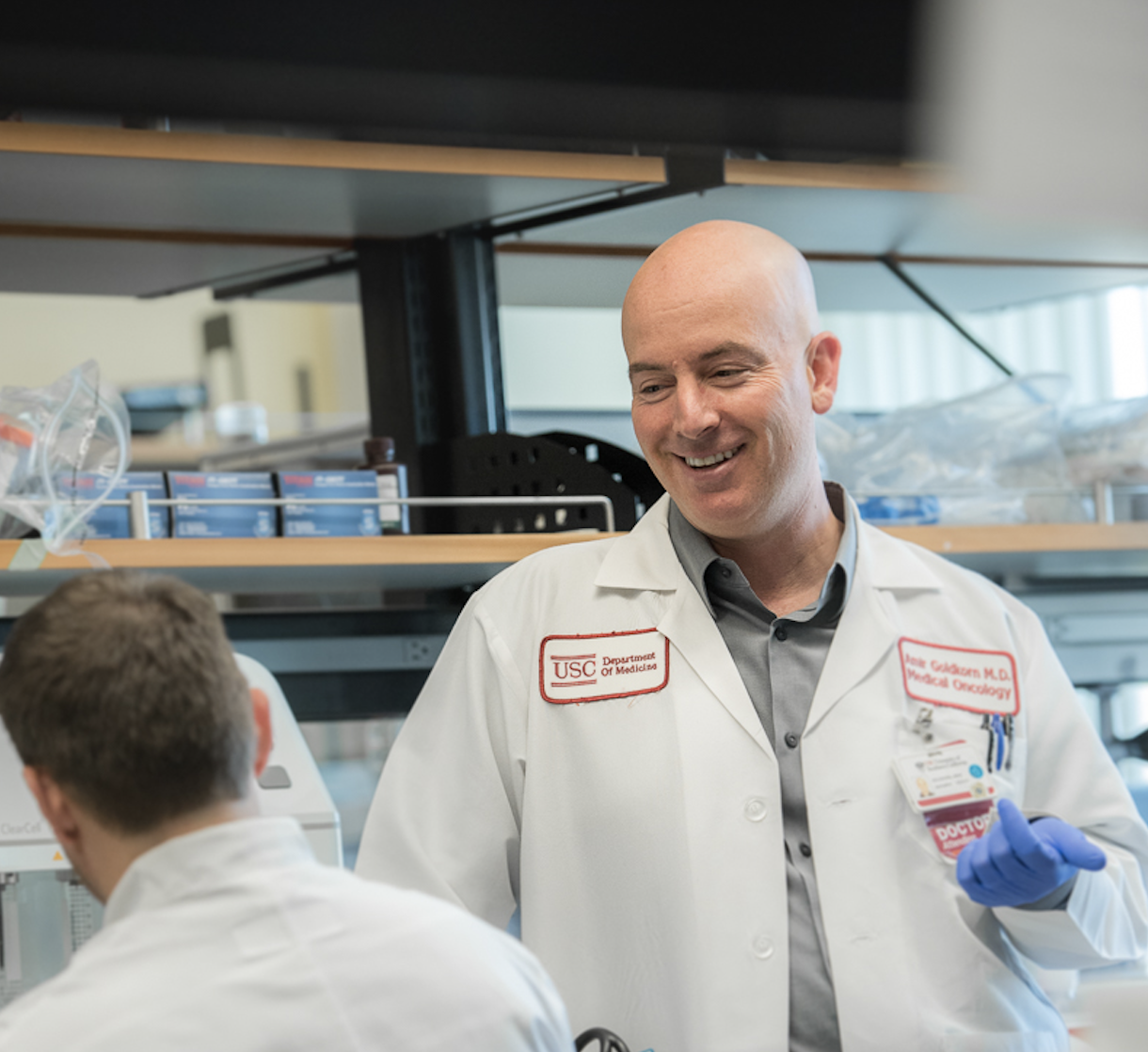
At the USC Norris Comprehensive Cancer Center, more than 250 dedicated physicians and scientists are leading the fight to make cancer a disease of the past. As one of the eight original National Cancer Institute-designated Comprehensive Cancer Centers in the United States, USC Norris has revolutionized cancer research, treatment, and prevention for nearly 50 years. Multidisciplinary teams provide the latest evidence-based care at USC Norris Cancer Hospital, a 60-bed hospital, as well as outpatient clinics throughout Los Angeles and Orange counties.
For more information, visit https://uscnorriscancer.usc.edu













 There are currently more than 3.8 million breast cancer survivors living in the U.S., yet three out of 10 women with invasive breast cancer will develop metastasis in their lifetime, meaning cancer that has spread to other organs. This is a source of worry for both patients and families. However, breast cancers that are not fully cured after treatment are often too small to be detected by mammograms or ultrasounds but pose a significant risk.
There are currently more than 3.8 million breast cancer survivors living in the U.S., yet three out of 10 women with invasive breast cancer will develop metastasis in their lifetime, meaning cancer that has spread to other organs. This is a source of worry for both patients and families. However, breast cancers that are not fully cured after treatment are often too small to be detected by mammograms or ultrasounds but pose a significant risk. 


 The
The