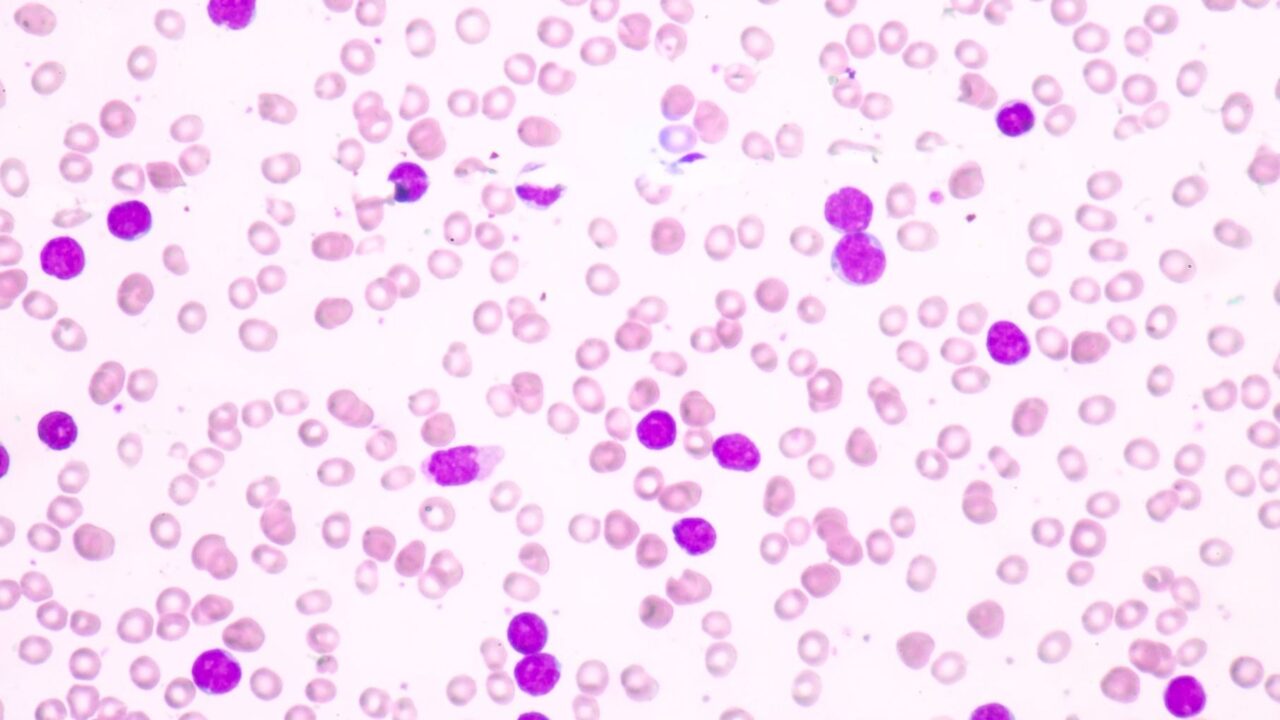
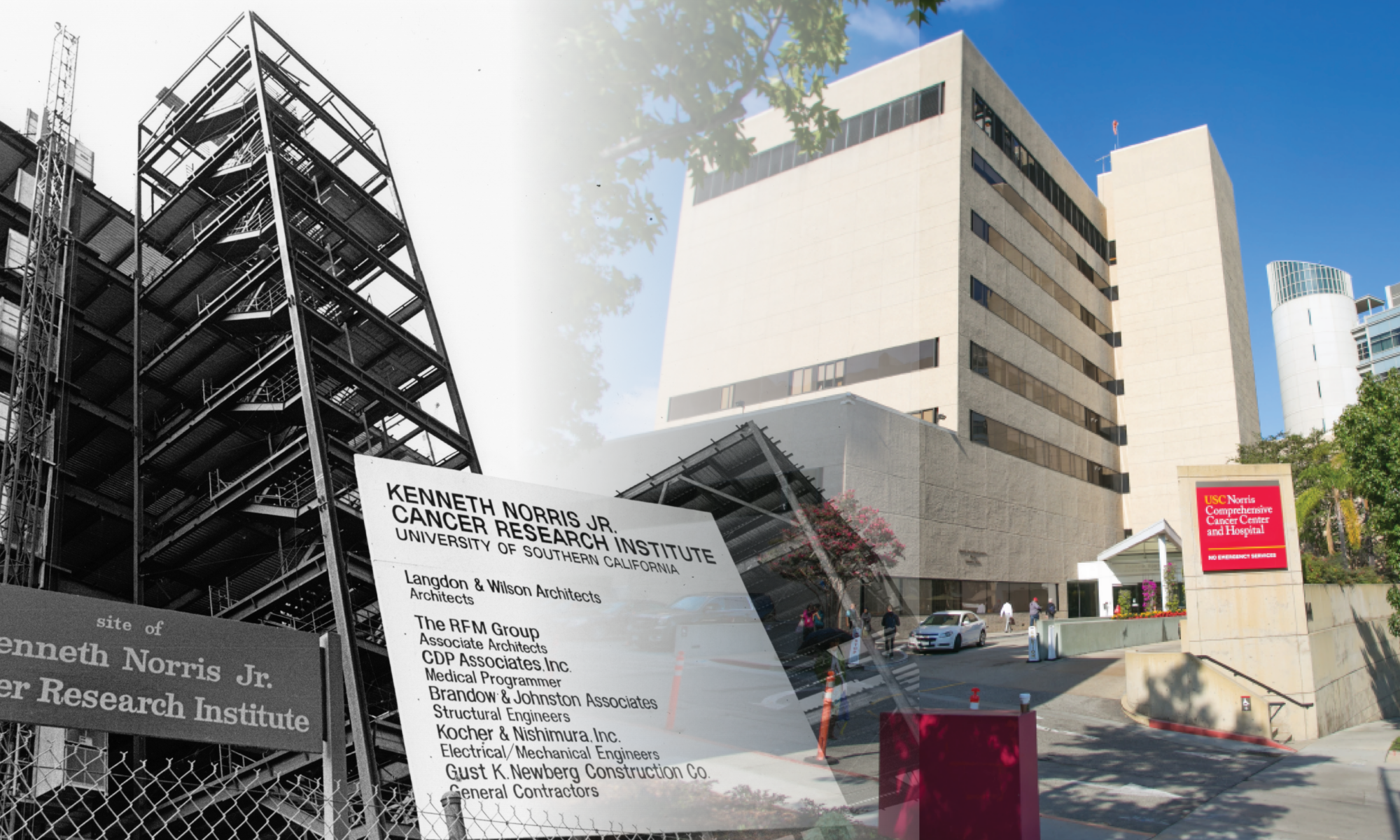
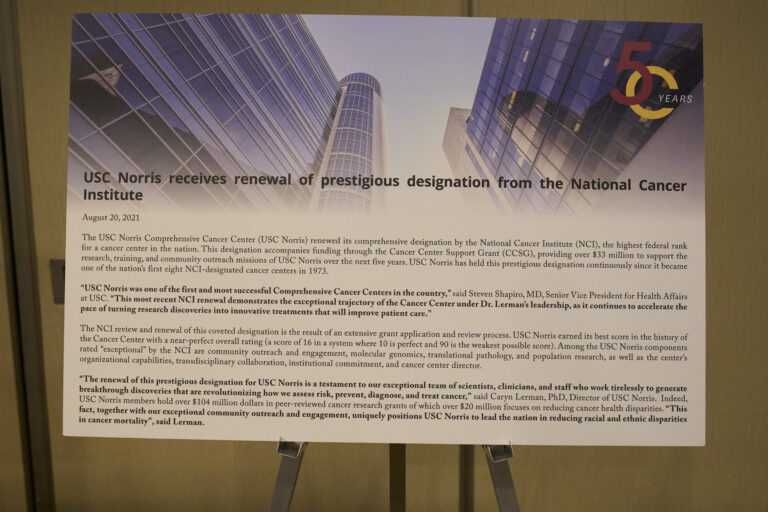
Register today for the 10th Annual Quinn Brady Memorial Swing Against Cancer Golf Tournament. This year’s event will benefit the USC Norris Comprehensive Cancer Center as well as Keck Medicine of USC’s Urology and Hematology divisions. Additionally, this year we have identified a local cancer center of excellence to support, Eisenhower Health Lucy Curci Cancer Center. All of these teams have one common goal: “KILL CANCER!” This event will be held in person at the La Quinta Country Club at 77-750 Avenue 50, La Quinta, California, on Monday, April 7, 2025. To register for the event, click the button above.
For more information or to register, please contact:
Bill Poland
Chair, Quinn Brady Memorial Swing Against Cancer Event
Phone: 310-291-7179
Email: bill@bill-poland.com