Large-scale study explores genetic link between colorectal cancer and meat intake
$20 million grant from the National Cancer Institute enables research into youth e-cigarette and oral nicotine use at USC
Study focusing on Black cancer survivors documents how exposure to racial discrimination impacts care
Mutations in 11 genes associated with aggressive prostate cancer identified in new research
USC Norris Comprehensive Cancer Center receives grant from The Ralph Lauren Corporate Foundation
33rd Festival of Life
Recent Posts
- USC researchers find genetic variant contributing to disparities in childhood leukemia risk
- Large-scale study explores genetic link between colorectal cancer and meat intake
- An Evening of Gratitude: Celebrating 50 Years
- $20 million grant from the National Cancer Institute enables research into youth e-cigarette and oral nicotine use at USC
- Swing Against Cancer 2024
USC Norris celebrates the courage and strength of their cancer survivors and families at the 33rd annual Festival of Life


The thundering sound of the USC Fight Song, piercing through the brass and percussion instruments of the USC Trojan Marching Band, signaled the beginning of the 33rd Festival of Life. The sound echoed throughout all of Pappas Quad at the Health Sciences Campus.
The event, held on the beautiful morning of Saturday, June 3, celebrated the strength, resilience, and tenacity of cancer survivors and their families. USC Norris Comprehensive Cancer Center and Hospital hosts this annual event, which included moving speeches from cancer survivors and an awe-inspiring dove release.
In keeping with tradition, the Tree of Life was installed near the check-in area, enabling attendees to honor loved ones who have survived, are currently battling, or have lost their lives to cancer by leaving uplifting words of survivorship. Additionally, patients and caregivers shared notes of appreciation with members of their support system from their cancer journey on the Festival of Life scroll.
W. Martin Kast, PhD, leader of the USC Norris Tumor Microenvironment Program and a professor of molecular microbiology and immunology, obstetrics and gynecology, and urology at the Keck School of Medicine of USC, served as master of ceremonies.The event included opening remarks by Steven Grossman, MD, PhD, the deputy director for Cancer Services at the USC Norris Cancer Center, and Joi Torrence-Hill, MHA, FACHE, the chief of hospital operations for the USC Norris Cancer Hospital.

“Surviving cancer is an extraordinary feat, one that demonstrates your unwavering strength, courage, and determination,” said Torrence-Hill. “Your journey has inspired countless others and serves as a beacon of hope for those who continue to fight. We are celebrating YOU, your triumphs, and the immense significance of this milestone in your lives.”
Huyen Q. Pham, MD, a gynecologic oncologist and director of the Gynecology/Oncology Clinic at Keck Medicine of USC, and an assistant professor of clinical obstetrics & gynecology at the Keck School, also spoke about updated information on treatment advances and new cancer research. In addition, Dr. Pham shared his experiences as a physician.
Cancer survivors, including Jared Lipscomb, a leukemia cancer survivor, and Julie Clauer, a colorectal cancer survivor, shared their cancer journeys, inspiring all those in attendance with their bravery, resilience, and strength.

“I know survivorship looks different for everyone, and I know survivorship is a gift not everyone receives, but I do believe that the moment we get that diagnosis, we become survivors,” said Jared. “Getting through a single round of chemo or radiation makes us survivors. Being able to hold on one more day makes us survivors. If this community has taught me anything, it is that strength can be found when you least expect it. Today’s celebration of survivorship is a reminder that each day is a gift, and I am so lucky and grateful to be here, alive and able to celebrate with all of you.”
Led by Judy Stark, a 22-year cancer survivor and volunteer at the cancer center and cancer hospital, and Awa Jones, chief nursing officer at the USC Norris Cancer Hospital, cancer survivors were invited to stand amid applause during the Festival of Life as a show of celebration and support. This tradition takes place every year at this event. Cancer survivors ranging from 20 years or more to those who are just beginning their survivorship were honored and received a roaring round of applause from all in attendance. Additionally, everyone in attendance at the Festival of Life applauded the patients currently undergoing treatment at USC Norris Cancer Hospital in a heartwarming, inspiring display of community and support.
The conclusion of the event was signaled by the annual tradition of the release of the doves. During this moment, the Bayou Brass Band played “Reach Out and Touch (Somebody’s Hand)” by Diana Ross. Doves are a symbol of hope, and by releasing the doves that day, attendees not only celebrated the cancer survivors and patients who battle their cancer every day, but also remembered those lost along the way.
“At USC we ‘Fight On.’ To all the cancer survivors out there, keep fighting on,” said Dr. Kast in his closing remarks.
USC research identifies biomarker that may predict treatment response to chemoimmunotherapy
Recent Posts
- USC researchers find genetic variant contributing to disparities in childhood leukemia risk
- Large-scale study explores genetic link between colorectal cancer and meat intake
- An Evening of Gratitude: Celebrating 50 Years
- $20 million grant from the National Cancer Institute enables research into youth e-cigarette and oral nicotine use at USC
- Swing Against Cancer 2024
USC research identifies biomarker that may predict treatment response to chemoimmunotherapy
Originally posted on Keck School of Medicine News
May 11, 2023
By Zara Abrams
The T-cell biomarker, which can be detected with a blood test, could help identify early in the treatment process which cancer patients will benefit from the combination of chemotherapy and immunotherapy and which are unlikely to see results.
 Cutting-edge cancer treatments like immunotherapy are offering new hope for patients, often in combination with more common approaches such as chemotherapy. But determining the best treatment combination isn’t always straightforward. Many patients spend valuable time on expensive therapies with serious side effects that aren’t effective against their cancer.
Cutting-edge cancer treatments like immunotherapy are offering new hope for patients, often in combination with more common approaches such as chemotherapy. But determining the best treatment combination isn’t always straightforward. Many patients spend valuable time on expensive therapies with serious side effects that aren’t effective against their cancer.
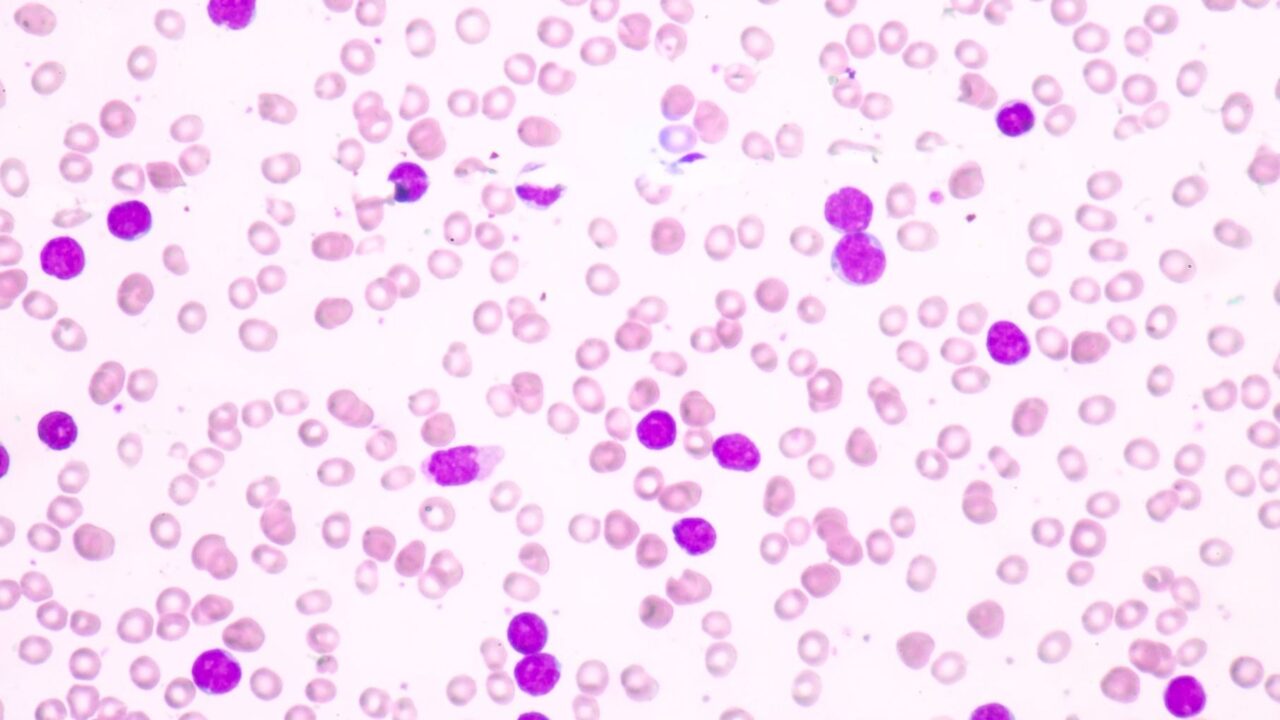
Now, a new discovery is poised to help. Researchers from USC Norris Comprehensive Cancer Center have identified a biomarker that indicates which patients with non-small cell lung cancer (NSCLC) will respond well to chemoimmunotherapy. The biomarker, known as CX3CR1, is expressed on T-cells and can be detected with a simple blood test, six to nine weeks after a patient starts treatment. The results were published in the journal Cancer Research Communications.
“We found that T-cell CX3CR1 expression can be used to monitor treatment effectiveness, and can be used as a biomarker to predict treatment response and prognosis for these patients,” said the study’s lead author, Fumito Ito, MD, PhD, associate professor of surgery at the Keck School of Medicine of USC and co-leader of the Translational and Clinical Science Research program at the USC Norris cancer center.
Ito and his team collected a series of blood samples from 29 patients with NSCLC who received a combination of immune checkpoint inhibitor (ICI) therapy and chemotherapy. They found that patients with elevated levels of CX3CR1 after six and nine weeks of treatment were more likely to see long-terms benefits from chemoimmunotherapy, including tumor shrinkage and cancer remission.
The findings build on earlier work by Ito and his team, published in 2021, which found that CX3CR1 can be used to predict treatment response in NSCLC patients receiving immunotherapy only. The biomarker may also be useful for other cancers and therapies and could ultimately help doctors and patients determine the most effective cancer treatments while avoiding unnecessary side effects and invasive biopsies.
An “early-on” treatment biomarker
ICI therapy has revolutionized the treatment of lung and other cancers, but it doesn’t work for all patients. For some, it can even trigger an autoimmune reaction marked by life-threatening problems with the lungs, liver, kidneys, or other organs.
Current pre-treatment methods to determine which patients will benefit from ICI therapy—and which will experience harmful side effects—don’t always work. CX3CR1 is the next best thing: an “early-on” treatment biomarker that is noninvasive. It can be measured when patients attend their first check-up and imaging appointment, typically about two months after starting ICI.
“If ICI is not working, we like to stop as soon as possible,” Ito said. “We have other viable treatment options for NSCLC patients, so the biomarker can help us identify patients who might have better results with an alternative therapy.”
Ito and his colleagues used a multi-omics approach, combining two cutting-edge sequencing methods to find the genomic and transcriptomic signature of T-cells. Each T-cell has a unique receptor pattern that can be used as a “barcode” to track them down in different parts of the body, including those attacking a tumor and those circulating in the blood.
“By combining two different types of next-generation sequencing, we found a way to characterize and monitor patients’ T-cells,” he said. “Next, we plan to use this analysis in a larger cohort to see if patients with other cancers will respond in a similar way.”
More evidence for CX3CR1
Because ICI therapy targets a patient’s immune system, rather than the tumor itself, the newly discovered biomarker could have broad utility across multiple types of cancer. In addition to testing other cancers, Ito and his colleagues also plan to explore whether CX3CR1 can predict treatment response to other types of immunotherapy, including adoptive T-cell therapy and vaccine-based therapy.
The team will also collect additional evidence for CX3CR1 in a larger group of non-small cell lung cancer patients undergoing ICI, both with and without chemotherapy. If additional research is successful, a blood test for the biomarker could reach broader patient populations in two to three years, Ito said.
About this study
In addition to Ito, the study’s other authors are Takayoshi Yamauchi from the Keck School of Medicine of USC; Eihab Abdelfatah from New York University Langone Health; and Mark D. Long, Ryutaro Kajihara and Takaaki Oba from the Roswell Park Comprehensive Cancer Center.
This work was supported by the Department of Defense Lung Cancer Research Program [LC180245], the National Cancer Institute [K08CA197966, R01CA255240-01A1, R01CA188900, R01CA267690, P30CA016056] and the Uehara Memorial Foundation.
New USC study shows immigrant adults with liver cancer have higher survival rates than those born in the US
Recent Posts
- USC researchers find genetic variant contributing to disparities in childhood leukemia risk
- Large-scale study explores genetic link between colorectal cancer and meat intake
- An Evening of Gratitude: Celebrating 50 Years
- $20 million grant from the National Cancer Institute enables research into youth e-cigarette and oral nicotine use at USC
- Swing Against Cancer 2024
New USC study shows immigrant adults with liver cancer have higher survival rates than those born in the US
By Hinde Kast
May 10, 2023
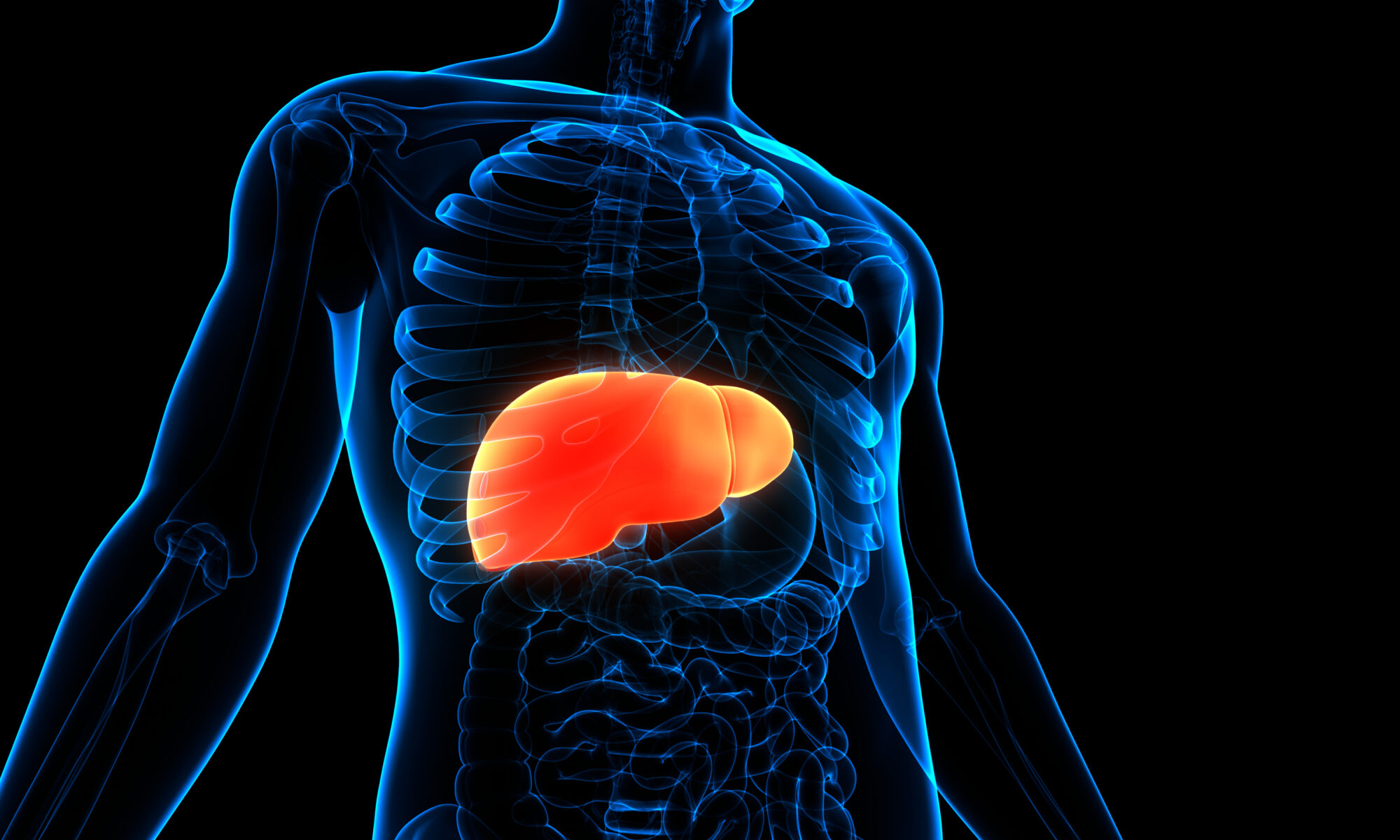
Immigrant adults with liver cancer in the United States have higher survival rates than people with the disease who were born in the U.S., according to new research from the USC Norris Comprehensive Cancer Center.
Hepatocellular carcinoma (HCC), the most common form of liver cancer, contributes to more than 27,000 deaths annually in the United States. Immigrants comprise a significant proportion of those diagnosed with HCC in the U.S. Research has shown that birthplace, also referred to as nativity, impacts incidence and risk factors for HCC, but little was known about its influence on survival after diagnosis.
The new study, just published in the Journal of the National Cancer Institute, identified a previously unrecognized disparity in survival after a diagnosis of liver cancer across all major racial/ethnic groups, with immigrants having better survival compared to those born in the U.S. This study is one of the first to robustly address nativity status as a predictor of overall survival for adults with HCC and provides important estimates of HCC survival by region of birth.
“Liver cancer is one of few cancers with increasing deaths. We identified a novel disparity by birthplace, whereby immigrants with liver cancer demonstrated better survival than their U.S.-born counterparts,” said study author Kali Zhou, MD, member of the Cancer Epidemiology Program at the USC Norris cancer center and a transplant hepatologist specializing in the treatment of chronic liver disease at Keck Medicine of USC. “This was true across different racial/ethnic groups. This finding is important as liver cancer rates are rising among U.S.-born and understanding why immigrants have better outcomes may help us create strategies to improve the survival of those born here.”
California has a high concentration of immigrants, representing about a quarter of the foreign-born population nationwide. This study used California Cancer Registry data to investigate whether birthplace impacts survival among patients with liver cancer, a cancer with poor prognosis that is common among immigrants, though rising in those born in the U.S.
Zhou, who is also an Assistant Professor of Clinical Medicine at the Keck School of Medicine of USC, and her colleagues identified 51,533 adults with HCC with available birthplace data in the California Cancer Registry between 1988 and 2017, of which 20,400 were people who were born in foreign countries. Cases were categorized as people who are born in the U.S. or people born in any other country, then stratified by four mutually exclusive race and ethnicity groups: Hispanic, non-Hispanic (NH) White, NH Black, and NH Asian/Pacific Islander. Results showed that 40% of all HCC cases were among those born outside of the U.S., and that their five-year survival rate was higher than patients with HCC who were born in the U.S. across all four major race and ethnicity groups. Among foreign-born people, lower mortality was observed in those from Central and South America compared to Mexico for Hispanics, East Asia compared to Southeast Asia for Asian/Pacific Islanders, and East Europe and Greater Middle East compared to West/South/North Europe for Whites.
The population-based California Cancer Registry provided a unique opportunity to compare HCC survival by nativity overall separated by regions of origin within individual race and ethnicity groups. Understanding the reasons for better survival among immigrants may help researchers address the disparity in survival rates by identifying ways to improve outcomes for people born in the U.S.
In addition to Kali Zhou, other contributors from the USC Norris Comprehensive Cancer Center and the Keck School of Medicine include Lihua Liu, PhD; Mariana Stern, PhD; Wendy Setiawan, PhD; Norah Terrault, MD, MPH; and Myles Cockburn, PhD.
This work was supported by the California Department of Public Health, the Centers for Disease Control and Prevention’s National Program of Cancer Registries, and the National Cancer Institute’s Surveillance, Epidemiology and End Results Program.
USC Norris collaborates with Auransa on clinical trial of new targeted treatment for liver cancer and other solid tumors
Recent Posts
- USC researchers find genetic variant contributing to disparities in childhood leukemia risk
- Large-scale study explores genetic link between colorectal cancer and meat intake
- An Evening of Gratitude: Celebrating 50 Years
- $20 million grant from the National Cancer Institute enables research into youth e-cigarette and oral nicotine use at USC
- Swing Against Cancer 2024
USC Norris collaborates with Auransa on clinical trial of new targeted treatment for liver cancer and other solid tumors
Dr. Anthony El-Khoueiry at the USC Norris Comprehensive Cancer Center will lead the phase 1 clinical trial of the novel drug AU409.
The University of Southern California (USC) is collaborating with Auransa Inc., on a phase 1 clinical trial to evaluate a new kind of treatment for cancers of the liver and solid tumors with liver dominant disease. The drug, known as AU409, was developed by Auransa, a clinical stage drug development company focused on identifying novel drug candidates for oncology, inflammatory diseases and diseases of the central nervous system. In preclinical trials, AU409, has been shown to work in a unique fashion by limiting the cancer cell’s ability to translate the message from various genes that are essential for the cancer cell’s ability to survive and multiply. In other words, AU409 interrupts the cancer cell’s machinery, preventing it from using DNA code to produce proteins that it needs to grow.
Liver cancer is estimated to be the third most common cause of cancer-related deaths worldwide, and hepatocellular carcinoma (HCC) accounts for about 80% of all liver cancers. Despite major improvements in treatment, patients with advanced HCC continue to have limited median overall survival due to primary or secondary resistance to existing therapies. While chronic hepatitis B and C infections continue to be important risk factors for liver cancer, the rising prevalence of obesity, non-alcoholic steatohepatitis (NASH), and alcohol consumption are becoming the dominant risk factors for liver cancer in the United States as well as the rest of the world.
The trial will involve patients from the USC Norris Comprehensive Cancer Center with advanced primary liver cancers or with advanced solid tumors with liver predominant metastatic disease. Its principal investigator is Dr. Anthony El-Khoueiry, a leading expert in early drug development for solid tumors, particularly gastrointestinal cancers. Dr. El-Khoueiry is the Director of the phase I program and Associate Director for Clinical Research at the USC Norris cancer center and Associate Professor of Clinical Medicine at the Keck School of Medicine of USC.
“We are excited at the potential impact our collaboration with Auransa can have for patients with solid tumors with liver predominant disease, in particular patients with hepatocellular cancer and cholangiocarcinoma. AU409 has a unique mechanism of action that impacts gene expression in the tumor and may represent a novel therapeutic approach for these tumors with high unmet need.” said Dr. El-Khoueiry.
“The collaboration with the USC Norris Comprehensive Cancer Center is an important first step in the clinical development of AU409 which is a new chemical entity with a unique mechanism of action. We plan to work closely with the team at USC to advance this very differentiated potential new drug for patients with liver cancers, specifically hepatocellular carcinoma (HCC), who may not respond to the currently available drugs.” said Pek Lum, Ph.D., co-founder and chief executive officer of Auransa.
“Dr. El-Khoueiry’s clinical trial experience spanning first-in-human, phase 2 and phase 3 trials, together with his interest in liver cancer, makes him the perfect lead of the AU409 clinical trial.” said Andrew Protter, Ph.D., Chief Scientific Officer of Auransa.
Auransa and USC are also collaborating on a broader approach to bring novel and much needed therapeutics to cancer patients, leveraging both Auransa’s proprietary artificial intelligence (AI) drug discovery platform to identify novel disease mechanisms and capabilities from the Rosalie and Harold Rae Brown Center for Cancer Drug Development at the USC Norris Comprehensive Cancer Center.
“The Brown Center for Cancer Drug Development takes an integrated academic-industry approach to achieve our mission of accelerating promising oncology therapeutics into the clinic through collaborative drug development,” said Caryn Lerman, PhD, director of USC Norris Comprehensive Cancer Center, and associate dean for cancer programs at the Keck School of Medicine at USC. “Together with Auransa, we are optimistic that we can develop new therapeutics for patients in need and further our mission.”
Disclosure: If this trial is successful, USC has the potential to receive royalty payments under the collaboration agreement with Auransa.
About University of Southern California’s Norris Comprehensive Cancer Center
The USC Norris Comprehensive Cancer Center (USC Norris), located in Los Angeles, is a major regional and national resource for cancer research, treatment, prevention, education, and community engagement. The National Cancer Institute (NCI) has designated the USC Norris Comprehensive Cancer Center as one of the nation’s 52 comprehensive cancer centers, a select group of institutions providing leadership in cancer treatment, research, prevention, and education. USC Norris has held this designation since 1973, at which time it was named as one of the first eight such centers in the country. The Rosalie and Harold Rae Brown Center for Cancer Drug Development (CCDD) at the USC Norris was launched in 2020 with a generous gift from the Rosalie and Harold Rae Brown Foundation. The CCDD employs an integrated academic-industry-focused management model to engage investigators from different disciplines, collapse gaps in expertise, resources, and funding, and ensure that programs have a high likelihood of progressing to the clinic.