Recent Posts
- Swing Against Cancer 2025
- New grant funds first-of-its-kind gene therapy to treat aggressive brain cancer
- Study links PFAS contamination of drinking water to a range of rare cancers
- USC study explores new insights into innate resistance for immunotherapies in colorectal cancer
- An early blood test can predict survival in patients with metastatic prostate cancer, shows USC study
University of Southern California Norris Comprehensive Cancer Center announces collaborative partnership with Sanford Burnham Prebys
August 2, 2021
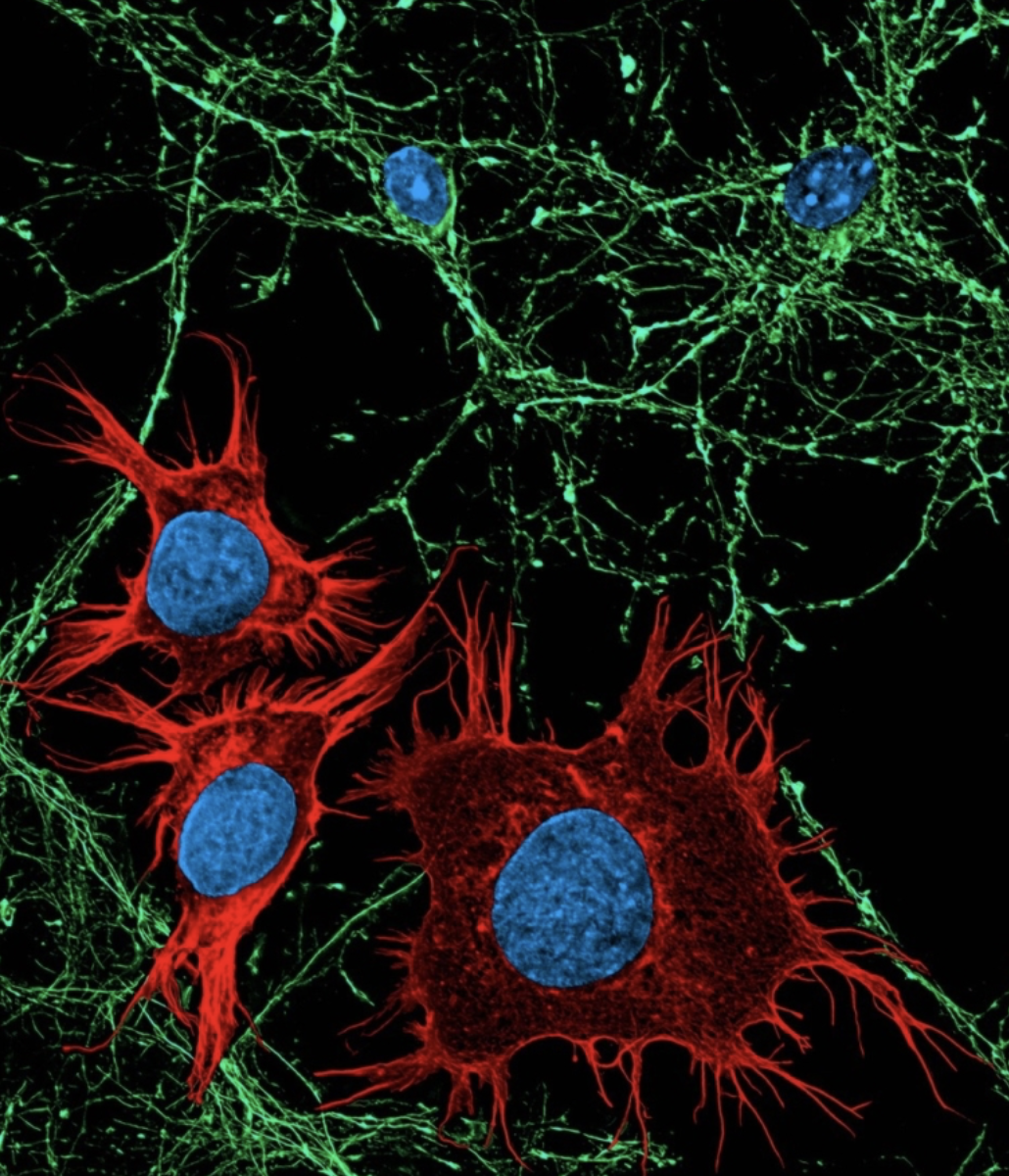
 To accelerate the development of groundbreaking cancer treatments, the Rosalie and Harold Rae Brown Center for Cancer Drug Development (CCDD) at the USC Norris Comprehensive Cancer Center at the Keck School of Medicine announces its first strategic partnership with Sanford Burnham Prebys.
To accelerate the development of groundbreaking cancer treatments, the Rosalie and Harold Rae Brown Center for Cancer Drug Development (CCDD) at the USC Norris Comprehensive Cancer Center at the Keck School of Medicine announces its first strategic partnership with Sanford Burnham Prebys.
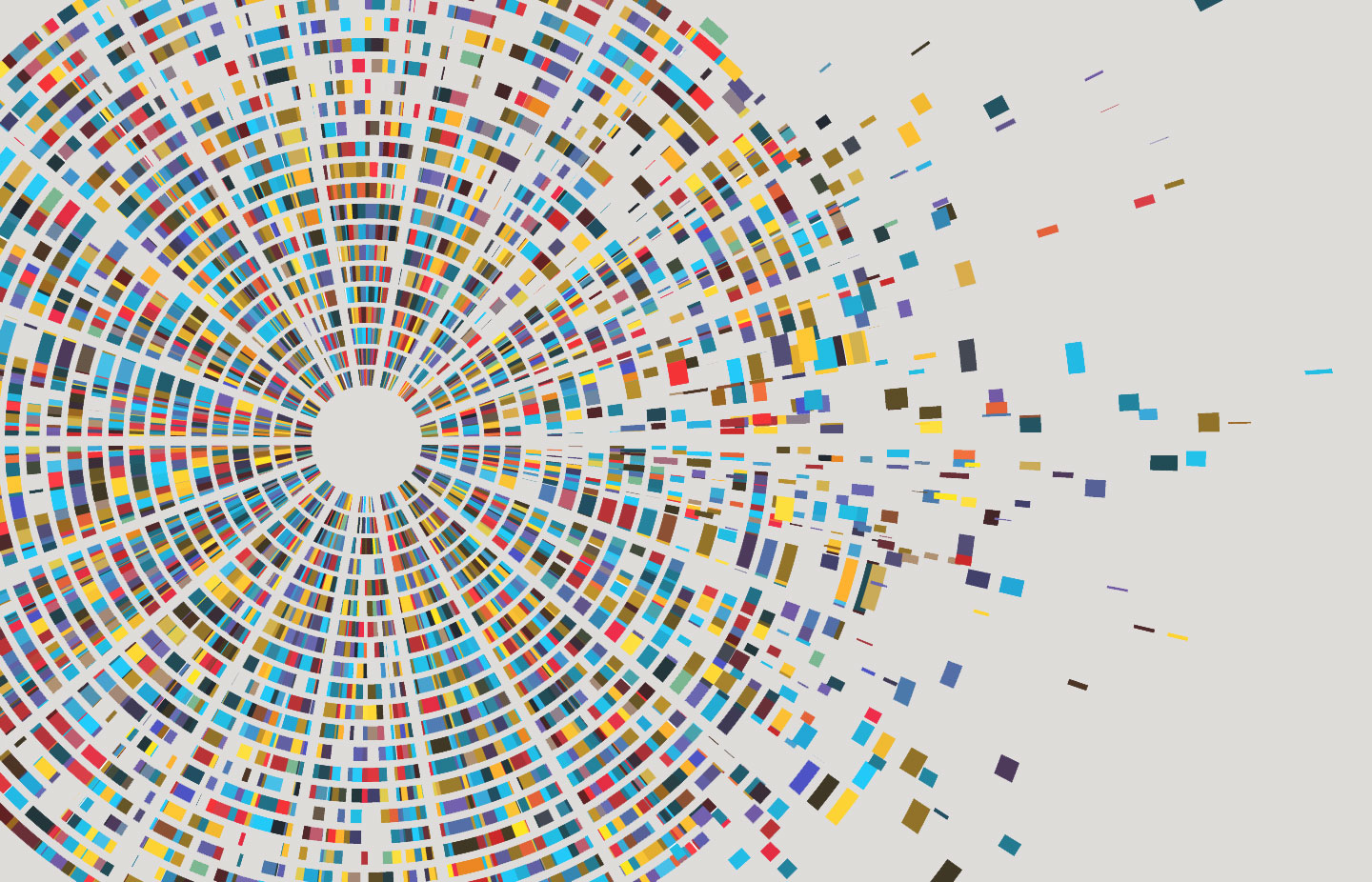
Under this agreement, USC researchers will collaborate with scientists at the Institute’s Conrad Prebys Center for Chemical Genomics (Prebys Center) to transition clinically relevant targets to early-stage drug discovery, including assay development and high-throughput screening to identify chemical compounds that modulate the activity of the targets. The Prebys Center is a comprehensive center for drug discovery and chemical biology and is fully equipped and staffed to conduct world-class drug discovery research. It includes a compound library with a collection of more than 1 million diverse chemicals. Validated “hits” from this library can be developed into prototype drugs.
“We are thrilled to have this opportunity to accelerate the development of new oncology therapeutics and ultimately bring new treatments and renewed hope to our patients,” said Caryn Lerman PhD, director of the USC Norris Comprehensive Cancer Center, H. Leslie and Elaine S. Hoffman Chair in Cancer Research, and associate dean for cancer programs in the Keck School of Medicine of USC.
Under the USC Norris Comprehensive Cancer Center, the partnership also establishes a joint steering committee that will review and prioritize projects considered for collaboration. This collaboration will provide a new innovation pathway for USC researchers to rapidly translate basic research discoveries into promising new therapeutics by closing the gaps in early-stage drug discovery resources and expertise.
“We’re looking forward to working with USC Norris to develop innovative screens to identify chemical compounds that modulate the activity of clinically relevant cancer targets,” said Michael Jackson PhD, senior vice president of drug discovery and development at Sanford Burnham Prebys. “If successful, these compounds will form the basis of entirely new—‘first in class’—therapies that can potentially improve the outcomes for people living with cancer.”
The partnership is open to all USC researchers interested in cancer drug discovery and serves as a critical resource for the recently established CCDD at the USC Norris Comprehensive Cancer Center. The mission of the CCDD is to accelerate promising oncology therapeutics into the clinic through collaborative drug development.
About USC Norris Comprehensive Cancer Center
At the USC Norris Comprehensive Cancer Center, more than 250 dedicated physicians and scientists are leading the fight to make cancer a disease of the past. As one of the eight original National Cancer Institute-designated Comprehensive Cancer Centers in the United States, USC Norris has revolutionized cancer research, treatment, and prevention for nearly 50 years. Multidisciplinary teams provide the latest research-based care at USC Norris Cancer Hospital, a 60-bed hospital, as well as outpatient clinics throughout Los Angeles and Orange counties.
For more information, visit https://uscnorriscancer.usc.edu
About Sanford Burnham Prebys Medical Discovery Institute
Sanford Burnham Prebys is a preeminent, independent biomedical research institute dedicated to understanding human biology and disease and advancing scientific discoveries to profoundly impact human health. For more than 40 years, our research has produced breakthroughs in cancer, neuroscience, immunology and children’s diseases, and is anchored by our NCI-designated Cancer Center and advanced drug discovery capabilities.
For more information, visit us at https:// SBPdiscovery.org










 Lourdes Baezconde-Garbanati, PhD, MPH, Associate Dean for Community Initiatives, was the recipient of the 2020 American Association for Cancer Research Distinguished Lectureship on the Science of Cancer Health Disparities.
Lourdes Baezconde-Garbanati, PhD, MPH, Associate Dean for Community Initiatives, was the recipient of the 2020 American Association for Cancer Research Distinguished Lectureship on the Science of Cancer Health Disparities.